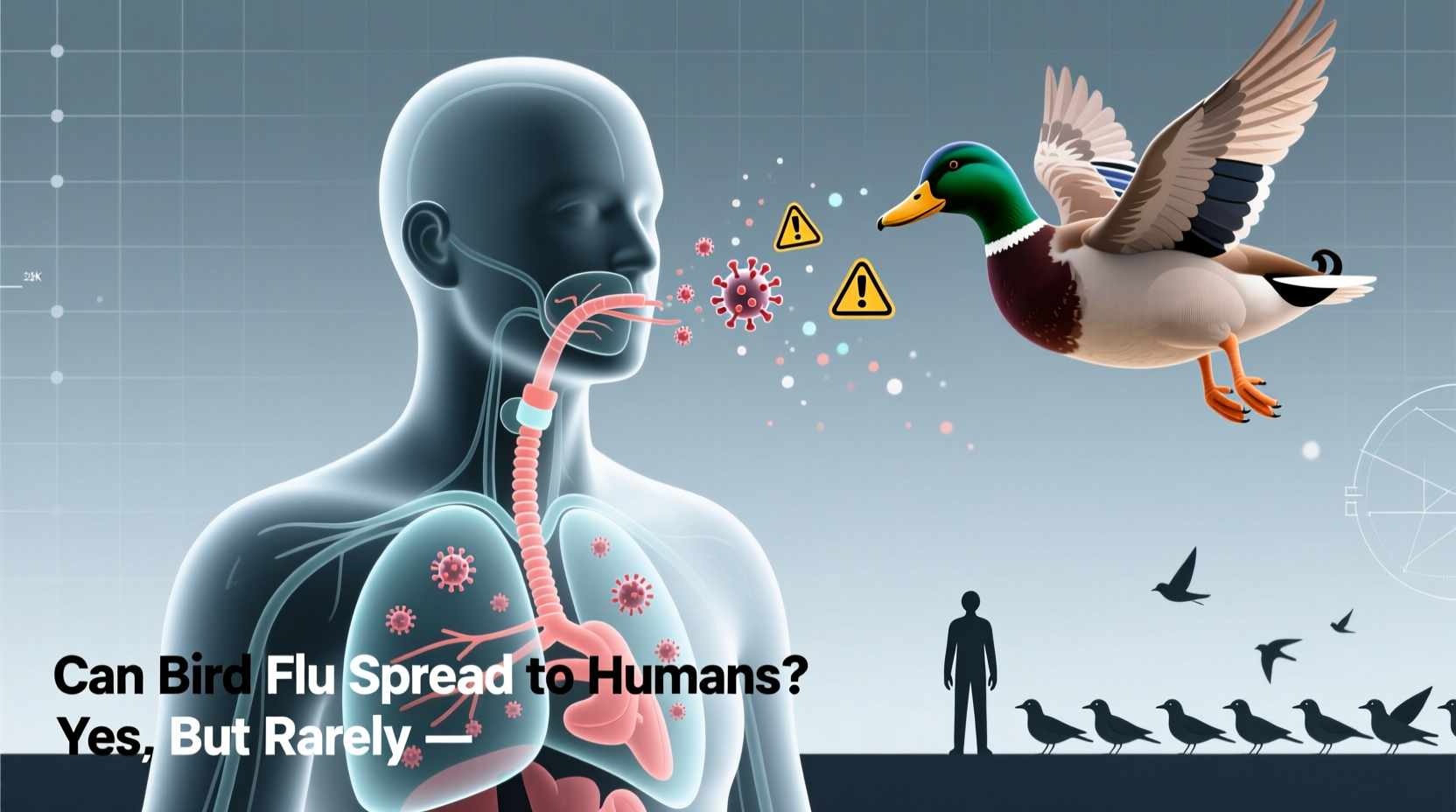
Yes, bird flu can spread to humans, although such transmissions are rare and typically occur under specific conditions. The most common way avian influenza spreads to people is through direct contact with infected birds or their droppings, especially in live poultry markets or during culling operations. While human-to-human transmission remains extremely limited, health organizations like the CDC and WHO closely monitor outbreaks due to the potential for the virus to mutate into a more contagious form. Understanding how bird flu jumps from birds to humans is crucial for prevention, especially for those working with poultry or engaging in wild bird observation.
Understanding Avian Influenza: Origins and Types
Bird flu, or avian influenza, refers to a group of influenza viruses that primarily infect birds. These viruses naturally circulate among wild aquatic birds, such as ducks and geese, which often carry the virus without showing symptoms. There are many strains of avian influenza, classified by surface proteins: hemagglutinin (H) and neuraminidase (N). Notable subtypes include H5N1, H7N9, and H5N6âall of which have caused sporadic infections in humans.
The H5N1 strain first emerged in 1996 in geese in China and gained global attention in 1997 when it infected 18 people in Hong Kong, six of whom died. Since then, over 900 human cases of H5N1 have been reported across more than 20 countries, with a fatality rate exceeding 50%. More recently, H5N1 has re-emerged in a highly pathogenic form affecting both commercial poultry and wild birds across North America, Europe, and Asia since 2021âraising renewed concerns about zoonotic transmission.
How Does Bird Flu Spread to Humans?
The primary route of bird flu transmission to humans involves close and prolonged exposure to infected birds. This includes handling sick or dead poultry, breathing in aerosolized particles from contaminated environments, or touching surfaces soiled with bird feces or saliva. Most human cases have occurred in individuals involved in farming, slaughter, or backyard poultry raising in regions experiencing outbreaks.
Itâs important to note that consuming properly cooked poultry or eggs does not pose a risk. The virus is destroyed at temperatures above 70°C (158°F), so standard cooking practices eliminate any threat. However, cross-contamination during food preparationâsuch as using unclean utensils or cutting boardsâcan still present a minor hazard if raw poultry juices come into contact with other foods.
Human-to-human transmission has only been documented in rare, isolated instances, usually involving close, unprotected contact with severely ill patients. No sustained community spread has ever been confirmed, but scientists remain vigilant because influenza viruses can rapidly evolve. If a strain acquired mutations allowing efficient person-to-person transmission, it could potentially trigger a pandemic.
Who Is at Risk of Contracting Bird Flu?
Certain populations face higher risks due to occupational or environmental exposure:
- Poultry workers: Farmers, transporters, slaughterhouse employees, and veterinarians working with flocks during an outbreak.
- Live market workers: Individuals in wet markets where live birds are sold, particularly in areas with poor biosecurity. \li>Wildlife researchers and bird handlers: Ornithologists, conservationists, and rehabilitators who handle wild birds.
- Travelers visiting affected regions: Especially those traveling to rural areas in countries experiencing active outbreaks.
Children and immunocompromised individuals may experience more severe illness if infected, though they are not necessarily more likely to contract the virus unless exposed to high-risk settings.
Symptoms of Bird Flu in Humans
Symptoms of avian influenza in humans can range from mild to life-threatening. Early signs resemble seasonal flu:
- Fever (often high)
- Cough
- Sore throat
- Muscle aches
- Headache
However, bird flu can progress rapidly to severe respiratory illness, including pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ failure. Some patients also report gastrointestinal symptoms such as diarrhea and vomiting. Because symptoms overlap with other respiratory infections, laboratory testingâincluding PCR assays on respiratory samplesâis required for definitive diagnosis.
Global Outbreaks and Surveillance Efforts
Since 2020, a new wave of H5N1 has swept across continents. In 2022, the United States recorded its largest-ever avian flu outbreak, affecting over 58 million birds across 47 states. Wild bird migrations have played a key role in spreading the virus, with detections in eagles, vultures, seals, and even dolphinsâindicating broader ecological impacts.
Internationally, countries including the UK, France, India, Japan, and South Korea have implemented mass culling and movement restrictions to contain outbreaks. The World Organisation for Animal Health (WOAH) and the Food and Agriculture Organization (FAO) coordinate global surveillance, urging transparency and rapid reporting from member nations.
In early 2024, the U.S. confirmed its first human case of H5N1 linked to dairy cow exposureâa novel development suggesting possible mammalian adaptation. Though the individual had only mild symptoms and recovered fully, this event marked a shift in understanding transmission dynamics and highlighted the need for expanded monitoring beyond poultry.
| Year | Location | Strain | Human Cases | Fatalities |
|---|---|---|---|---|
| 1997 | Hong Kong | H5N1 | 18 | 6 |
| 2003â2004 | Asia (multiple) | H5N1 | ~100 | ~50 |
| 2013 | China | H7N9 | 1,568 | 616 |
| 2022â2024 | Global (including U.S.) | H5N1 | ~60 | ~20 |
Prevention and Safety Measures
For the general public, the risk of contracting bird flu remains low. However, taking precautions is essential for those in high-exposure roles. Key preventive strategies include:
- Avoid contact with sick or dead birds: Do not touch or attempt to rescue wild birds showing signs of illness (e.g., lethargy, inability to fly).
- Use personal protective equipment (PPE): Gloves, masks (N95 or equivalent), goggles, and disposable gowns should be worn when handling birds or cleaning enclosures.
- Practice strict hygiene: Wash hands thoroughly with soap and water after any potential exposure. Disinfect tools and surfaces used around birds.
- Report unusual bird deaths: Contact local wildlife authorities or agricultural departments if you find clusters of dead birds.
- Stay informed about local outbreaks: Check updates from national health agencies such as the CDC or your countryâs public health ministry.
Myths and Misconceptions About Bird Flu
Several myths persist about avian influenza, leading to unnecessary fear or complacency:
- Myth: Eating chicken gives you bird flu. Fact: Properly cooked poultry is safe. The virus cannot survive high heat.
- Myth: Bird flu spreads easily between people. Fact: Sustained human-to-human transmission has never been observed.
- Myth: Only chickens carry the virus. Fact: Wild waterfowl are natural reservoirs, and recent cases show infection in mammals like foxes, seals, and cows.
- Myth: A vaccine exists for all strains. Fact: While experimental vaccines exist for some strains (like H5N1), none are widely available to the public. Seasonal flu shots do not protect against avian influenza.
What Should Birdwatchers Know?
For birdwatchers and nature enthusiasts, the risk of contracting bird flu is minimalâbut responsible practices help protect both human and avian health. Follow these guidelines:
- Maintain distance from wild birds; use binoculars instead of approaching.
- Do not feed waterfowl in areas with known outbreaks.
- Clean boots, gear, and vehicle tires after visiting wetlands or farms.
- Avoid bringing pet birds into areas frequented by wild populations.
- Participate in citizen science programs that report sick or dead birds to authorities.
Future Outlook and Research Directions
Scientists are actively studying how avian influenza evolves and crosses species barriers. Genomic sequencing helps track mutations that could enhance transmissibility or virulence. Researchers are also exploring universal flu vaccines that might offer protection across multiple strains, including avian variants.
Additionally, improved biosecurity on farms, better surveillance in wild bird populations, and international cooperation are critical to preventing large-scale outbreaks. Climate change and habitat loss may further influence bird migration patterns, potentially altering the geographic spread of the virus.
Frequently Asked Questions (FAQs)
- Can I get bird flu from watching birds in my backyard?
- No, simply observing birds from a distance poses no risk. Avoid handling birds or cleaning feeders without gloves if outbreaks are reported locally.
- Is there a treatment for bird flu in humans?
- Yes. Antiviral medications like oseltamivir (Tamiflu) can reduce severity if administered early. Hospitalization may be needed for severe cases.
- Are pets at risk of getting bird flu?
- Cats can become infected if they eat infected birds, though cases are rare. Keep cats indoors during outbreaks. Dogs appear less susceptible.
- Has bird flu ever caused a pandemic?
- No. Despite several zoonotic outbreaks, no strain has achieved efficient and sustained human-to-human transmission necessary for a pandemic.
- How can I tell if a bird has avian flu?
- Sick birds may show tremors, twisted necks, difficulty breathing, or sudden death. However, many infected birds die suddenly without visible signs. Always assume dead birds could be infectious.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4