Influenza is not inherently bird flu, but certain types of influenza viruses originate in birds—specifically avian influenza, commonly known as bird flu. The term 'influenza' encompasses a broad family of viruses that infect various species, including humans, pigs, and birds. However, when people ask, 'is influenza a bird flu,' they are often referring to whether all flu comes from birds or if human flu is the same as avian flu. The answer is no: while some strains of influenza have origins in birds, seasonal human influenza is primarily caused by different subtypes adapted to spread among people. Avian influenza, particularly strains like H5N1 and H7N9, can occasionally jump from birds to humans, causing severe illness, but sustained human-to-human transmission remains rare.
Understanding Influenza and Its Origins
Influenza viruses belong to the Orthomyxoviridae family and are categorized into four main types: A, B, C, and D. Among these, Influenza A is the most diverse and significant in terms of zoonotic potential—the ability to jump between animals and humans. This type includes subtypes defined by two surface proteins: hemagglutinin (H) and neuraminidase (N). There are 18 known H subtypes and 11 N subtypes, many of which circulate predominantly in wild aquatic birds such as ducks, geese, and shorebirds.
These birds serve as natural reservoirs for avian influenza viruses, typically carrying them without showing symptoms. The virus spreads through feces, saliva, and nasal secretions, contaminating water sources and environments where other birds congregate. While most avian influenza strains cause mild disease in wild birds, some evolve into highly pathogenic forms—such as H5N1—that can devastate poultry populations and pose risks to humans.
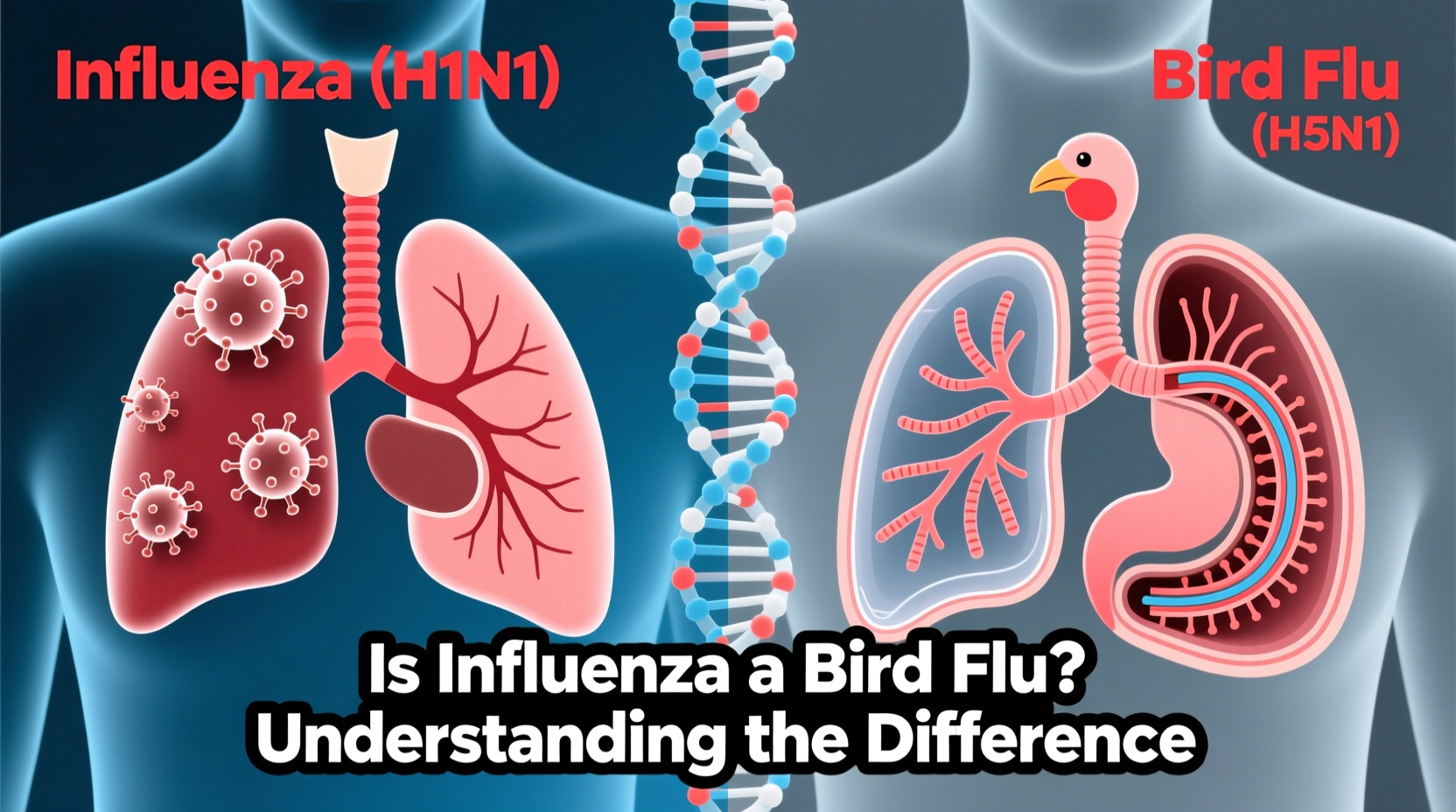
Differentiating Between Human Flu and Bird Flu
A common misconception arises from conflating seasonal flu with bird flu. Seasonal influenza in humans is mainly driven by Influenza A(H1N1), A(H3N2), and Influenza B viruses that circulate annually and are transmitted efficiently between people via respiratory droplets. These strains have adapted over time to human immune systems and are responsible for annual flu epidemics.
In contrast, avian influenza does not easily transmit between humans. When human infections occur, they are usually linked to direct contact with infected birds or contaminated environments—such as live poultry markets or farms experiencing outbreaks. Symptoms in humans can range from mild conjunctivitis to severe pneumonia and multi-organ failure, depending on the strain.
For example, since its emergence in 1997, the H5N1 strain has caused over 900 confirmed human cases globally, with a case fatality rate exceeding 50%, according to the World Health Organization. Despite this severity, widespread human transmission has not occurred, limiting pandemic risk under current conditions.
Historical Context: Major Outbreaks and Global Impact
The relationship between influenza and birds became globally apparent during several pivotal outbreaks. One of the earliest recognized instances was the 1997 Hong Kong outbreak of H5N1, where six people died after exposure to infected chickens. This prompted mass culling of poultry and heightened surveillance worldwide.
Another notable event was the global spread of H5N1 beginning in 2003, which moved from Asia to Europe and Africa through migratory bird pathways. More recently, an unprecedented wave of highly pathogenic avian influenza (HPAI) began in 2021–2022, affecting millions of commercial and backyard birds across North America, Europe, and parts of Africa and Asia. In the U.S. alone, over 58 million birds were culled or died due to H5N1 during the 2022 outbreak, marking it one of the largest animal health emergencies in history.
This resurgence raised concerns about viral evolution and spillover into mammals—including foxes, seals, sea lions, and even dairy cattle in early 2024—suggesting possible adaptation toward broader host ranges.
Biological Mechanisms: How Bird Flu Spreads
Avian influenza spreads primarily through direct contact with infected birds or indirect exposure to contaminated surfaces and materials. Wild waterfowl play a crucial role in long-distance dissemination, shedding the virus in their droppings into lakes and wetlands used by domestic flocks. Once introduced into poultry farms, especially those with poor biosecurity, the virus can spread rapidly.
The distinction between low pathogenic avian influenza (LPAI) and high pathogenic avian influenza (HPAI) lies in the virus’s ability to cause disease. LPAI strains may only cause mild respiratory signs or reduced egg production in chickens, whereas HPAI strains trigger rapid organ failure and death in up to 90–100% of infected birds within days.
Mutations in the hemagglutinin protein allow certain LPAI viruses to convert into HPAI forms, often after circulating undetected in poultry populations. This evolutionary shift underscores the importance of monitoring and early detection programs.
Human Risk and Public Health Implications
While human infections remain sporadic, public health agencies closely monitor avian influenza due to its pandemic potential. If an avian strain gains the ability to transmit efficiently between humans, it could lead to a global outbreak, especially since populations lack pre-existing immunity.
To assess risk, scientists examine viral genetic sequences for mutations associated with mammalian adaptation, such as changes in the polymerase complex (PB2-E627K mutation) or receptor binding specificity (switching preference from avian-type alpha-2,3 sialic acid receptors to human-type alpha-2,6). Detection of such markers raises alarms and triggers enhanced surveillance.
Currently, antiviral drugs like oseltamivir (Tamiflu) are effective against most avian influenza strains if administered early. Vaccines for specific strains, such as H5N1, exist but are stockpiled rather than widely distributed, reserved for emergency use in case of a pandemic.
Practical Advice for Bird Owners and the General Public
For backyard poultry keepers and small-scale farmers, preventing avian influenza starts with strong biosecurity practices:
- Limit visitors’ access to bird areas.
- Disinfect footwear and equipment before entering coops.
- Avoid sharing tools or transporting birds between flocks unnecessarily.
- Provide feed and water in enclosed areas to prevent contamination by wild bird droppings.
- Report sudden bird deaths or signs of illness (lethargy, swelling, decreased egg production) to local veterinary authorities immediately.
During active outbreaks, government agencies may impose movement restrictions or temporary bans on live bird markets. Staying informed through official agricultural departments or wildlife health networks is essential.
For general travelers visiting regions with ongoing avian flu activity, avoiding contact with live poultry markets and ensuring poultry products are thoroughly cooked (>165°F internal temperature) reduces infection risk. There is no evidence of transmission through properly handled and cooked food.
Regional Differences in Surveillance and Response
Responses to avian influenza vary significantly by country based on agricultural infrastructure, regulatory capacity, and ecological factors. In the European Union, strict monitoring and mandatory reporting protocols help contain outbreaks quickly. In contrast, resource-limited countries may face delays in diagnosis and response, increasing the likelihood of undetected spread.
In the United States, the USDA’s Animal and Plant Health Inspection Service (APHIS) coordinates national surveillance, offering diagnostic support and compensation for depopulated flocks. Canada operates a similar system through the Canadian Food Inspection Agency (CFIA).
In Asia, where live bird markets are culturally and economically important, interventions focus on market hygiene improvements, periodic rest days, and zoning to separate species. However, enforcement challenges persist.
| Region | Surveillance System | Response Strategy |
|---|---|---|
| North America | National labs, real-time PCR testing | Culling, quarantine, movement controls |
| European Union | Centralized reporting, EU Reference Lab | Compensation, biosecurity mandates |
| Southeast Asia | Market-based surveillance | Hygiene upgrades, vaccination (limited) |
| Africa | Limited lab capacity, reliance on OIE | Emergency response only |
Debunking Common Misconceptions
Several myths surround avian influenza. One is that eating chicken or eggs can give you bird flu. As previously noted, proper cooking destroys the virus, making consumption safe. Another myth is that pet birds are major carriers; while possible, household parrots or canaries are far less likely to be exposed unless in contact with wild birds or infected poultry.
Additionally, some believe that all bird die-offs are due to avian flu. In reality, numerous diseases, toxins, and environmental stressors can cause mass mortality. Confirmation requires laboratory testing.
Future Outlook and Preparedness
As climate change alters migratory patterns and intensifies farming practices increase animal density, the interface between wild birds, domestic poultry, and humans continues to expand—raising the probability of viral spillover events.
Investments in global surveillance, rapid diagnostics, and universal influenza vaccines offer promising avenues for reducing future risks. International collaboration through organizations like the WHO, FAO, and WOAH (World Organisation for Animal Health) remains critical.
For individuals, staying informed through reliable scientific sources—not social media rumors—is key. Monitoring updates from national health and agriculture agencies ensures timely awareness of local threats.
Frequently Asked Questions
- Can humans get bird flu from watching wild birds?
No, simply observing birds at a distance poses no risk. Transmission requires close contact with infected birds or contaminated materials. - Is there a vaccine for bird flu in humans?
Yes, pre-pandemic vaccines exist for strains like H5N1 and are held in strategic stockpiles, but they are not available to the general public. - Does bird flu affect all bird species equally?
No. Waterfowl often carry the virus without symptoms, while chickens and turkeys are highly susceptible to severe disease. - Can dogs or cats get bird flu?
Rare cases have been reported, usually following ingestion of infected birds. Most pets face minimal risk under normal circumstances. - How is bird flu detected in birds?
Veterinarians collect swabs from the cloaca and trachea, then use RT-PCR tests to identify viral RNA in laboratories.










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4