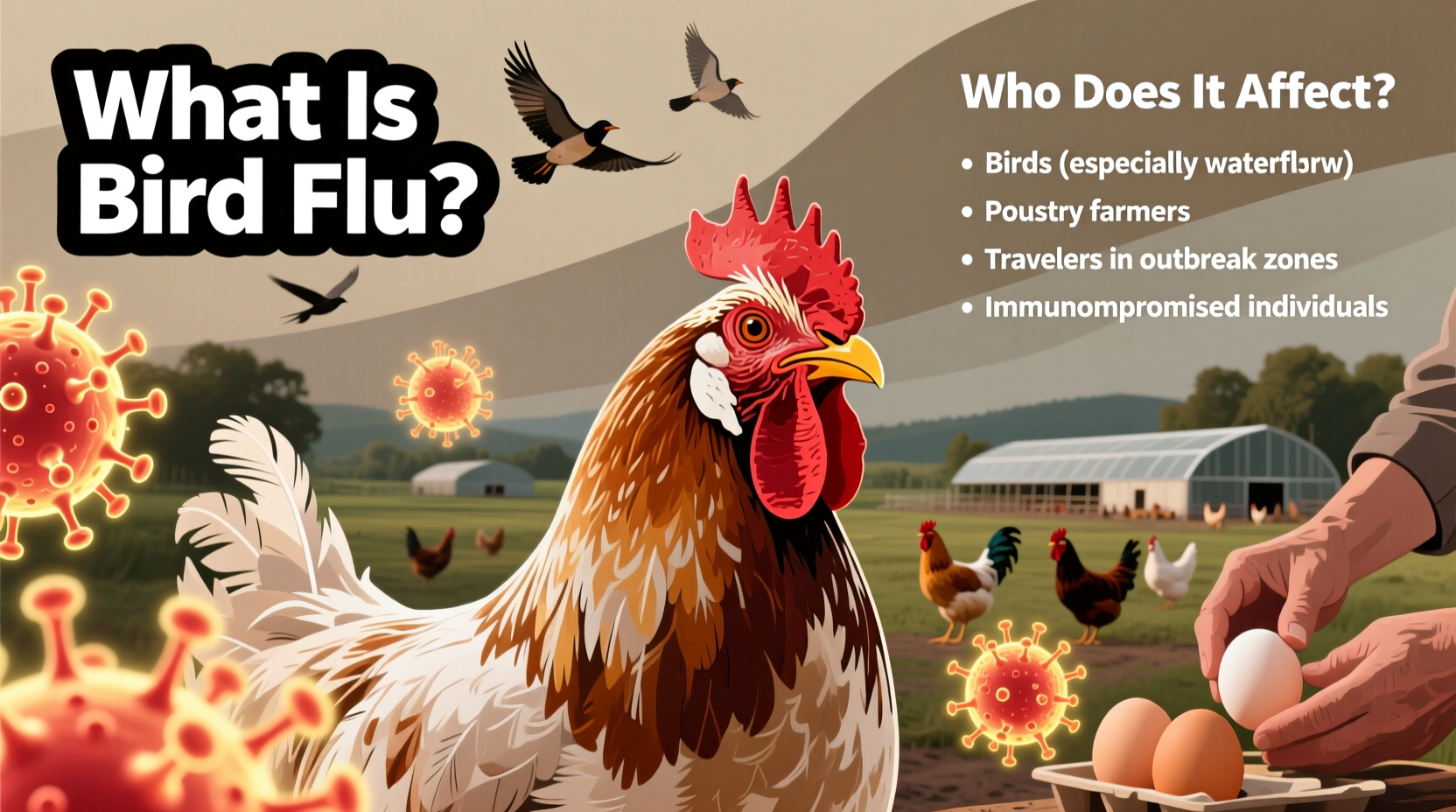
Bird flu, also known as avian influenza, is a viral infection that primarily affects birds, including both wild and domesticated species. The term 'who bird flu' often refers to inquiries about the causes, transmission, and impact of this disease, particularly in relation to human health and global outbreaks. Avian influenza viruses belong to the influenza A family and are naturally hosted by wild aquatic birds such as ducks, geese, and shorebirds, which can carry the virus without showing symptoms. These birds play a critical role in the global spread of the virus through migration patterns, making surveillance essential for early detection and containment.
Understanding the Biology of Bird Flu
The causative agents of bird flu are influenza A viruses, classified based on two surface proteins: hemagglutinin (H) and neuraminidase (N). There are 18 known H subtypes and 11 N subtypes, but the most concerning strains for both animal and human health include H5N1, H7N9, and H5N8. These viruses are highly contagious among birds and can lead to high mortality rates in poultry populations. While most avian influenza strains do not easily infect humans, certain variants like H5N1 have caused severe illness and death in people who had close contact with infected birds.
Transmission occurs mainly through direct contact with secretions from infected birds, such as saliva, nasal discharge, and feces. Contaminated surfaces, equipment, and water sources also serve as vectors. In rare cases, limited human-to-human transmission has been reported, though sustained spread between people remains uncommon. This biological behavior underscores why public health agencies monitor outbreaks closely, especially in regions where humans live in close proximity to backyard flocks or live bird markets.
Historical Outbreaks and Global Impact
The first major recorded outbreak of highly pathogenic avian influenza occurred in Italy in 1878, although it wasn't until the late 20th century that modern virology identified the specific strains involved. One of the most significant events was the emergence of the H5N1 strain in Hong Kong in 1997, when six people were infected and two died. This marked the first time bird flu was shown to directly jump from birds to humans, prompting widespread culling of poultry and intensified global surveillance.
Since then, multiple waves of H5N1 have spread across Asia, Africa, Europe, and more recently, North America. In 2022, an unprecedented panzootic (animal pandemic) of H5N1 affected over 77 countries, leading to the death or culling of more than 150 million birds. The 2024–2025 season continues to see active circulation of clade 2.3.4.4b H5N1, with detections in wild birds, commercial farms, and even marine mammals such as seals and sea lions—raising new concerns about cross-species adaptation.
Cultural and Symbolic Significance of Birds in Relation to Disease
Birds have long held symbolic meaning across cultures—from messengers of the divine in ancient Greece to omens of change in Indigenous traditions. However, during bird flu outbreaks, these cultural perceptions shift dramatically. In some rural communities, migratory birds once celebrated for their seasonal return are now viewed with suspicion. Poultry, central to many cuisines and rituals, becomes a source of fear rather than sustenance.
In parts of Southeast Asia, where cockfighting and free-range farming are common, efforts to control bird flu face resistance due to economic dependence and deep-rooted practices. Similarly, in West Africa, traditional beliefs about animal spirits sometimes delay reporting of sick birds, complicating containment. Public education campaigns must therefore balance scientific messaging with cultural sensitivity to ensure compliance with biosecurity measures.
How Bird Flu Affects Humans: Risk Factors and Symptoms
While human infections remain rare, they are often severe. Most cases occur in individuals who handle live or dead infected birds, work in poultry processing, or visit live bird markets. Symptoms typically appear within 2 to 8 days after exposure and may include fever, cough, sore throat, muscle aches, and conjunctivitis. In severe cases, pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ failure can develop.
As of mid-2025, the World Health Organization (WHO) has confirmed fewer than 900 human cases of H5N1 since 2003, with a case fatality rate exceeding 50%. Despite this high lethality, there is no evidence of efficient human-to-human transmission. Ongoing research focuses on whether genetic mutations could enable easier spread, which would raise pandemic potential. For now, the risk to the general public remains low, provided standard precautions are followed.
Prevention and Biosecurity Measures
Preventing bird flu requires coordinated action at individual, national, and international levels. Key strategies include:
- Surveillance: Monitoring wild bird populations and poultry farms for signs of infection.
- Biosecurity: Implementing strict hygiene protocols on farms, including disinfecting equipment, limiting visitor access, and isolating new birds.
- Vaccination: Although vaccines exist for poultry, they are used selectively to avoid masking infections and interfering with trade.
- Public Awareness: Educating communities about safe handling of birds and reporting sick or dead wildlife.
In households with backyard flocks, simple steps like keeping feed covered, avoiding contact with wild birds, and washing hands after handling chickens can significantly reduce risk. Hunters should wear gloves and masks when field-dressing game birds and avoid consuming meat from animals that appeared ill.
Role of Migration in Spreading Bird Flu
Migratory birds are central to the ecology of avian influenza. Species such as the bar-headed goose, ruddy shelduck, and various shorebirds travel thousands of miles annually along flyways that span continents. During migration, they congregate in wetlands and stopover sites, creating ideal conditions for virus transmission.
Climate change is altering migration timing and routes, potentially increasing overlap between wild birds and domestic flocks. Warmer temperatures may also extend the survival of the virus in the environment. Satellite tracking and genetic sequencing of virus samples help scientists trace outbreak origins and predict future hotspots. International cooperation through organizations like the Food and Agriculture Organization (FAO) and the Global Avian Influenza Network for Surveillance (GAINS) enhances early warning systems.
Current Status and Regional Differences in 2025
As of early 2025, bird flu activity remains elevated worldwide. In North America, the United States Department of Agriculture (USDA) reports ongoing detections in commercial turkey and egg-laying operations, particularly in the Midwest. Canada has seen increased mortality in wild raptors and scavengers feeding on infected carcasses.
In Europe, the European Centre for Disease Prevention and Control (ECDC) notes a decline in spring 2025 compared to peak winter months, but warns of possible resurgence in autumn. Meanwhile, parts of East Asia continue to experience sporadic outbreaks despite routine vaccination programs in poultry.
These regional differences reflect variations in farming density, climate, surveillance capacity, and policy responses. For example, countries with centralized poultry industries can implement rapid depopulation and movement controls, while smallholder systems face greater challenges in enforcement.
| Region | Key Strain | Primary Hosts | Human Cases (2020–2025) |
|---|---|---|---|
| North America | H5N1 clade 2.3.4.4b | Wild waterfowl, turkeys, dairy cattle* | 2 (both mild) |
| Europe | H5N1 | Wild birds, farmed ducks | 0 |
| East Asia | H5N6, H7N9 | Poultry, live markets | 12 (including fatalities) |
| Africa | H5N1 | Migratory birds, village chickens | 5 (under investigation) |
*Note: Recent studies suggest possible transmission between infected birds and dairy cattle, raising new zoonotic concerns.
Common Misconceptions About Bird Flu
Several myths persist about avian influenza:
- Myth: Eating properly cooked poultry or eggs can give you bird flu.
Fact: The virus is destroyed at cooking temperatures above 70°C (158°F). Safe food handling eliminates risk. - Myth: All bird flu strains are deadly to humans.
Fact: Most strains do not infect humans; only a few, like H5N1 and H7N9, pose serious threats. - Myth: Bird flu spreads easily between people.
Fact: Sustained human-to-human transmission has not been documented.
What Travelers and Birdwatchers Should Know
For birdwatchers and ecotourists, bird flu does not necessitate avoiding nature, but caution is advised. Avoid touching sick or dead birds and report them to local wildlife authorities. Use binoculars instead of approaching nests or roosts. Clean boots and gear after visiting wetlands to prevent spreading pathogens.
Travelers to areas with active outbreaks should avoid live bird markets and poultry farms. Check advisories from national health departments before visiting rural regions in affected countries. No travel restrictions are currently in place, but awareness helps prevent accidental exposure.
Future Outlook and Research Directions
Ongoing research aims to improve diagnostics, develop universal avian influenza vaccines, and enhance predictive modeling using AI and satellite data. Scientists are also investigating the role of environmental factors—such as nutrient runoff and habitat loss—in amplifying disease transmission.
Given the interconnectedness of ecosystems, agriculture, and human health, addressing bird flu requires a One Health approach—integrating veterinary, medical, and environmental expertise. Investment in global surveillance infrastructure remains crucial to preventing spillover events and preparing for potential pandemics.
Frequently Asked Questions (FAQs)
- Can pets get bird flu?
- Cats can become infected if they eat raw infected birds, but dog infections are extremely rare. Keep cats indoors during outbreaks.
- Is it safe to feed wild birds in my backyard?
- During active outbreaks, consider pausing bird feeders. If used, clean them weekly with a 10% bleach solution and remove spilled seed.
- Has bird flu ever caused a human pandemic?
- No. While H5N1 is highly lethal, it lacks efficient human-to-human transmission. It is not considered a pandemic threat at this time.
- How is bird flu different from seasonal flu?
- Seasonal flu circulates among humans and is caused by H1N1 or H3N2. Bird flu originates in birds and rarely infects people.
- Where can I find real-time bird flu updates?
- Reliable sources include the WHO, USDA Animal and Plant Health Inspection Service (APHIS), and the European Food Safety Authority (EFSA).










 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4